Addiction & Mental Health
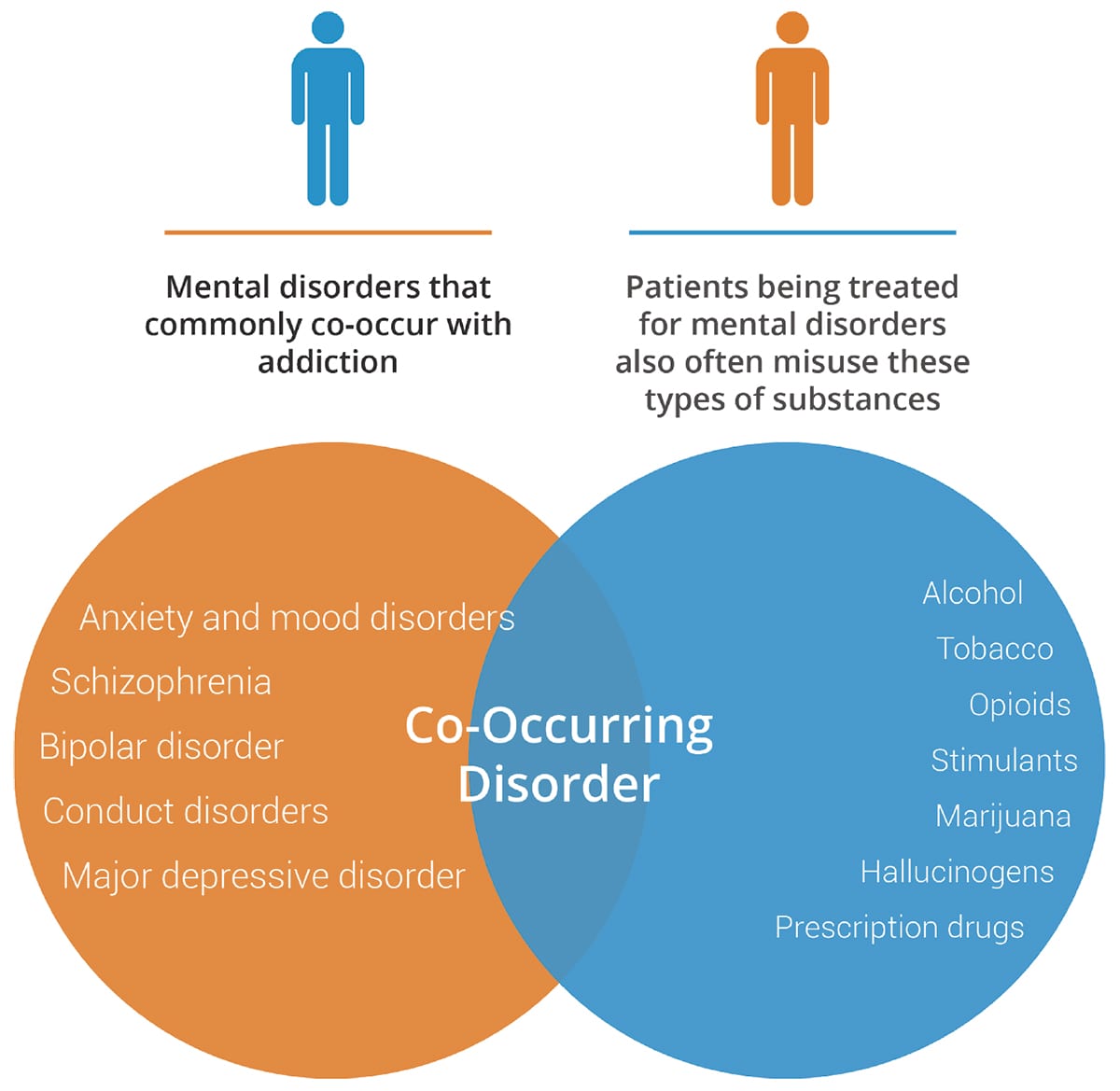
Co-occurring is also called comorbidity or dual diagnosis—when two disorders or illnesses occur in the same person, simultaneously or one after another. Comorbidity also implies that the illnesses interact, affecting the course and prognosis of both. 1
Co-occurring conditions that involve addiction and mental health are common because similar areas of the brain are involved with both. About 50% of people with a mental health issue will also experience a substance use disorder and vice versa. 2
What causes co-occuring disorders?
Research has shown that mental illness and drug use involve similar areas of the brain. The areas of the brain that process “reward” feelings and that respond to stress are both affected by mental health disorders and by using drugs.
Drug use affects the brain and can aggravate the symptoms of existing mental health conditions. Often, someone with a mental health condition may try to self-medicate by treating symptoms of anxiety or depression by using alcohol or drugs. While the substances may give temporary relief, when they wear off, their symptoms are often much worse.

According to the National Survey on Drug Use and Health (2018), 9.2 million adults in the U.S. experienced both mental illness and a substance use disorder.
The Stigma of Drug Addiction
Belittling terms such as alcoholic, drunk, junkie, or crackhead perpetuate stigma and negatively affect a person’s self-esteem, damage relationships and prevent someone from getting access to the care they really need.
They suffer in shame, guilt, and embarrassment, terrified to find themselves in this situation. The initial decision to take drugs is usually voluntary, but with on-going use, drugs change the brain in ways that make quitting very difficult even for someone
who wants to stop.
Studies show people who enter drug treatment programs as a result of loving pressure do better in treatment than those who are shamed or humiliated. At PHCA, we know addiction is not a choice. It’s not a moral failing, it doesn’t only happen to “weak”
people, and it’s not a character flaw.
What do addiction and mental health disorders have in common?
Genetics
Development
Exposure
Emotional signs of stress can include:
- Depression
- Anxiety
- Irritability
- Mood Swings
- Compulsive behavior
- Memory & concentration problems
How are co-occuring disorders treated?
The best treatment for co-occurring disorders is to take an integrated approach that addresses both the person’s diagnosed mental health condition and addiction. Successful treatments include behavioral therapies and medications, used together as part of a personalized plan.
1 NIDA https://www.drugabuse.gov/publications/research-reports/common-comorbidities-substance-use-disorders/introduction
2 SAMHSA https://www.samhsa.gov/medication-assisted-treatment/treatment/common-comorbidities
3 NIDA https://www.drugabuse.gov/publications/drugfacts/comorbidity-addiction-other-mental-disorders
Rather than focusing soley on a person’s misuse of drugs, we treat the WHOLE PERSON
